Q: How can I best manage the ventilation in my own office/school/home?
A: Scientists are calling for more attention to VENTILATION in prevention of SARS-CoV-2 transmission.
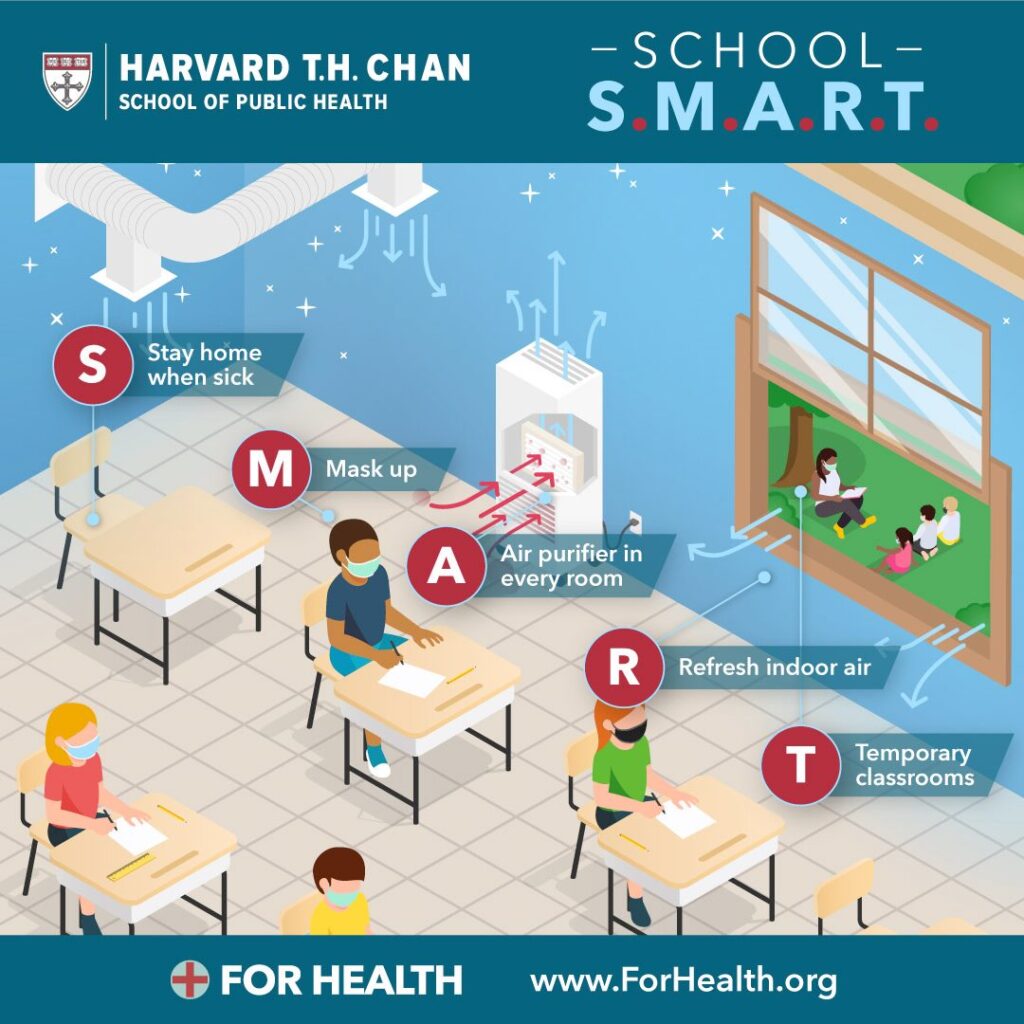
You can help manage risk by opening doors and windows where possible, increasing outside airflow and filtration in HVAC systems, using portable HEPA air filters, and wearing masks indoors.
As ever, try to avoid crowded, poorly ventilated indoor spaces.
While there has been debate from scientists from different disciplines regarding the terminology of “droplets” vs “aerosols,” the take home message remains that the virus is primarily transmitted through breathing in expelled virus from an infected person–many of whom may be asymptomatic or pre-symptomatic and thus not visibly ill.
See our previous post on the “is the virus airborne?” kerfuffle.
Because of the dominance of airborne transmission in SARS-CoV-2, we may be focusing too much on sanitizing surfaces (a recent article aptly named this phenomenon “hygiene theatre”) and not enough on the AIR around us.
SARS-CoV-2 reproduces in our respiratory tract and is emitted when we breathe, talk, sing, cough, or sneeze. The SIZE of the infectious particles is key for understanding different types of transmission risk.
Droplets, as the name suggests, are larger particles that are heavy enough to mostly drop to the ground with the recommended 3-6 feet of social distancing. Aerosols, on the other hand, are more like a fine mist that can travel in the air for longer distances and accumulate in enclosed spaces.
In reality, there is no true dichotomy between droplets and aerosols, and we emit particles of sizes that vary along this continuum from large to small. But evidence for the role of smaller aerosols has been growing.
So, can you contract the virus from walking into the room where an infected person has recently been? Not likely, but *possible* if the room is small and stuffy.
Can the virus travel via air ducts or pipes? Again, this is theoretically possible, but thus far there is no evidence of transmission of SARS-CoV-2 via air ducts.
In fact, SARS-CoV-2 seems to NOT behave like the most contagious airborne pathogens such as measles, where one infected person’s emissions can travel to the far reaches of buildings and cause infection (THANKFULLY!)
The practical consequences of smaller aerosol transmission are that indoors, physically distancing by itself may not be as effective as we assumed. While it is true that *most* of the particles are concentrated around the infected person, they can also accumulate and get around a room. Because of this, increased ventilation and masks are highly recommended indoors regardless of physical distancing.
So, how do we best minimize transmission risk in contexts where people gather?
1.) DILUTE: Where possible, dilute viral particles’ presence by exchanging air in the room with air from outside (and thus lowering the dose, which matters for the possibility and the severity of infection). Many building-wide air-conditioning systems have a setting for how much air they take in from outside, which can be cranked up to dilute the air and minimize re-circulation of air.
2.) FILTER: When windows cannot be opened, rooms could run portable HEPA filters, which are capable of trapping viruses (no fancy add-ons needed). Upgrade filters in the HVAC system to MERV 13 or higher.
3.) GET OUTSIDE: Where feasible, get outside including setting up canopies/tents. While clearly a different era, teaching moved outdoors during the 1918 pandemic.
4.) WEAR MASKS: Masks help block aerosols released by the wearer. Scientific evidence is also building that masks protect the wearer from breathing in aerosols around them.
Finally, we recognize the constraints many schools and other venues face in meeting these ventilation goals in old buildings or in climates not conducive to outdoor activities. Funding to help upgrade systems and purchase filters or accommodations for outdoor activities is desperately needed as part of our national prevention efforts.
For further scientific details, please read this excellent article by Zeynep Tufecki and from Dr. Lindsay Marr.