A recent large study of U.S. Veterans found that the risk of having a heart attack, stroke and a long list of other cardiovascular events was higher for those who had COVID-19 the year prior compared to those who didn’t. The risk was highest for those who had been admitted to the hospital or ICU but was still elevated for those not hospitalized.
🙋 How much higher was the risk? Should I be worried? ….it’s complicated.
While the overall news was not good, this Nerdy Girl was very happy to see the authors express the increased risk in both *relative* and *absolute* terms. What’s the difference?
The relative risk is often what we see in alarming headlines—for example in this study the risk of a heart attack was 63% higher in those who had COVID-19. Sounds bad, right? The relative risk tells us that risk is higher in one group compared to another, but it doesn’t tell us the whole story.
To put relative risk in perspective, we also need to know the absolute risk of the bad thing happening.
➡️ An example: In a group of 100,000 people, 1 might develop a rare cancer. In people who get a lot of x-rays, perhaps this risk goes up to 2 people out of 100,000. In this example, the relative risk of cancer is DOUBLE (2 ÷1) for those getting the x-rays (making for a scary headline), but the absolute risk difference is very small–only 1 extra person out of 100,000 gets cancer.
➡️ Compare that to a case where 10,000 out of 100,000 typically develop this cancer and x-rays again DOUBLE the risk. That means 20,000 out of 100,000 people getting lots of x-rays will get the cancer. The relative risk is still 2 (20,000 ÷ 10,000), but now *10,000* more people out of 100,000 will get cancer compared to only 1 additional person in the previous scenario.
⁉️ That’s weird…this seems like a big difference in interpretation?!
Yes and no–neither of these numbers is wrong, but the different perspectives highlight how the numbers you choose to present can make a story seem more or less dramatic. For this Nerdy Girl, relative and absolute risks are best used together, so kudos to the authors for clear and transparent communication of their results (see figure).
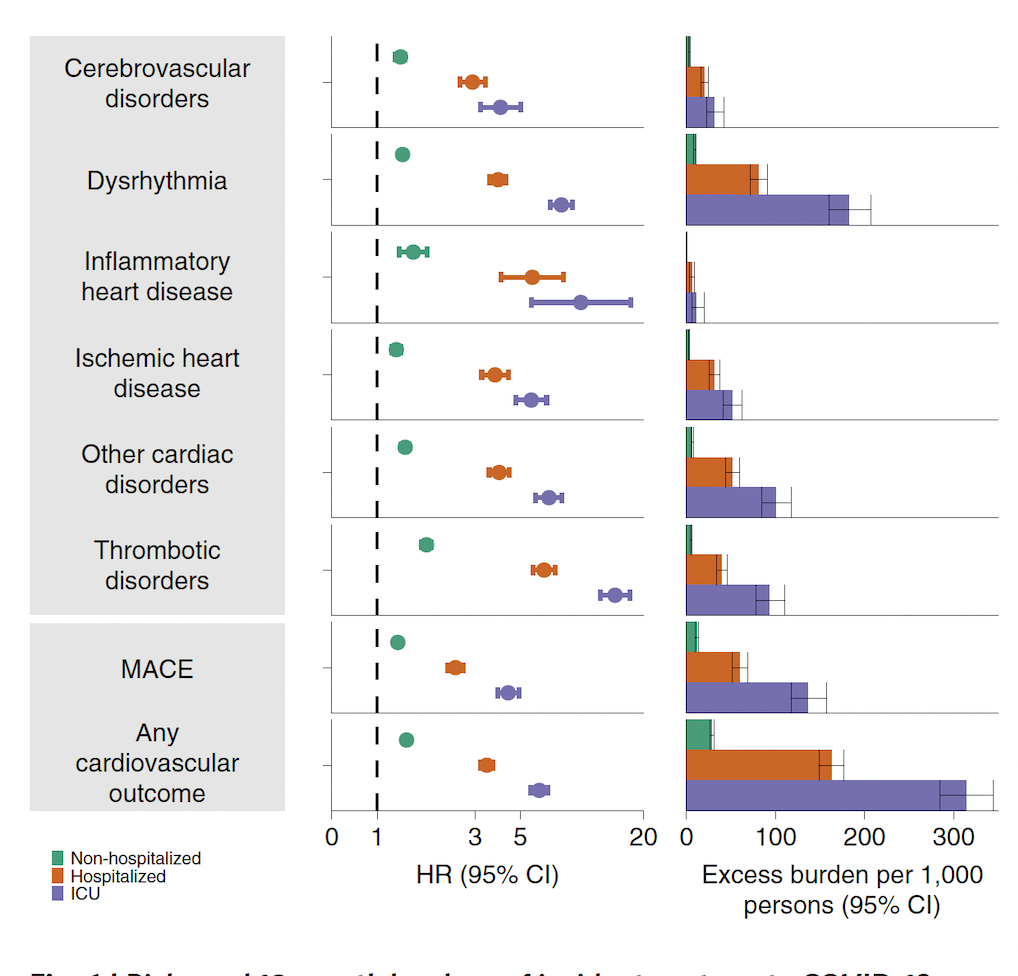
The study looked at over 20 different cardiovascular outcomes, but we can go back to the finding of a 63% higher risk of having a heart attack (a.k.a myocardial infarction) over a year for those who had COVID-19. This relative increase corresponds to a heart attack risk of 4.67/1000 for the control group (no-COVID) compared to 7.59/1000 for those who had COVID-19 in the previous year. So, in absolute terms, an extra 3 people out of 1000 had a heart attack after having COVID-19 compared to the group not having COVID-19.
❓Is this effect big or small? It depends how you look at it.
With tens of millions of people getting infected with COVID-19, an increase of 3 heart attacks for every thousand people can add up fast. For some of the other outcomes the absolute risk was larger. At the population level, this could lead to a noticeable rise in cardiovascular disease burden.
At the individual level, most people’s risk of having a heart attack in the next year is quite low (thankfully!) As in the first cancer example, if you double a low risk….it is still a low risk.
⬇️ BOTTOM LINE:
These results are concerning. This was a well-designed study showing evidence that COVID-19 likely raises the risk of a variety of cardiovascular events after infection. We don’t fully understand the biological mechanisms, but hypotheses include direct viral invasion of cardiac and endothelial cells, inflammation, and/or scarring of the heart tissue. Whatever the mechanism, given the huge number of infections globally, this is bad news.
But at the individual level, you don’t need to panic. The results do NOT mean that if you have had COVID-19 you have a high risk of heart problems. That absolute risk is still low (and of course depends on many other risk factors).
❇️ While this study did not look at vaccination, the highest risk was in those hospitalized or in the ICU. The vaccines are highly effective at preventing severe disease and hospitalization, meaning it’s very likely vaccines would reduce this risk substantially (though this is a topic for future research).
➡️ We shouldn’t need more reasons to avoid infection and get vaccinated, but accumulating evidence of long term health effects of COVID-19 is certainly *extra* motivation.
Stay Safe and Stay Sane!
Love,
Those Nerdy Girls
Study Summary:
“Heart-disease risk soars after COVID — even with a mild case”
Full study:
“Long-term cardiovascular outcomes of COVID-19”
Figure Legend:
“Composite outcomes consisted of cerebrovascular disorders (stroke and TIA), dysrhythmias (atrial fibrillation, sinus tachycardia, sinus bradycardia, ventricular arrhythmias and atrial flutter), inflammatory heart disease (pericarditis and myocarditis), ischemic heart disease (acute coronary disease, myocardial infarction, ischemic cardiomyopathy and angina), other cardiac disorders (heart failure, non-ischemic cardiomyopathy, cardiac arrest and cardiogenic shock), thrombotic disorders (pulmonary embolism, deep vein thrombosis and superficial vein thrombosis), MACE (all-cause mortality, stroke and myocardial infarction) and any cardiovascular outcome (incident occurrence of any cardiovascular outcome studied). Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up.”


