A. Although the reasons for the disparities are numerous and complex, a few of our posts this week point to potential targets for intervention (e.g. segregation, healthcare system, and others).
Clinicians and scientists have also offered data and policy solutions to address the high burden COVID-19 infections, hospitalizations, and deaths that are disproportionately impacting minority communities.
Some of these include:
1. Improve the systematic collection and quality of data on race and ethnicity. This is necessary “to ensure that prevention and treatment interventions reach those most in need.”
2. Offer free and equitable access to COVID-19 testing without restrictions. Requiring a doctor’s order for testing or offering only drive-through options limits access to people who don’t have a regular doctor or who don’t have a car.
3. Increase health insurance access and coverage. A large proportion of Americans, but especially Black and Latino families, have lost health insurance due to COVID-19 related job losses. This creates enormous financial obstacles to seeking treatment.
4. Direct funding towards community-based organizations responding to the pandemic in Black and Latino neighborhoods. This allows for more informed implementation of interventions.
5. Offer timely public health communication in multiple languages and in a manner that’s culturally appropriate. COVID-19 misinformation is as big of an issue in underserved communities, and is perhaps even more harmful, because of the high risk of infection and death they face.
For more information on these and other recommendations:
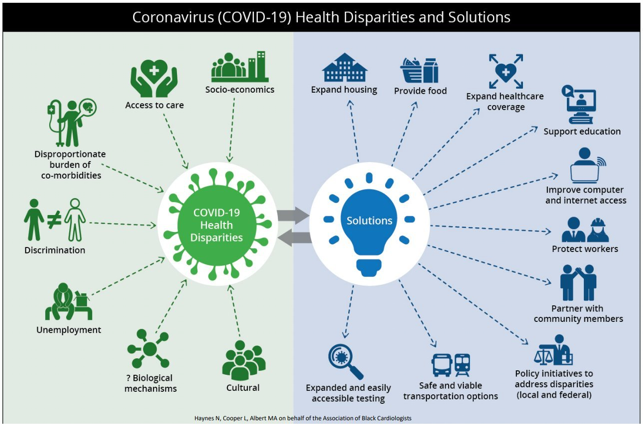
The Association of Black Cardiologists has also created a graphic to help visualize some of the reasons underlying race/ethnic disparities in COVID-19 with potential solutions (see photo).
Photo credit: Haynes N, Cooper L, Albert MA. At the Heart of the Matter: Unmasking and Addressing COVID-19’s Toll on Diverse Populations. Circulation 4 May 2020.