Q: It seems like COVID-19 can have some short and long-term effects on the brain. What is the likelihood that psychiatric issues will arise in COVID-19 survivors?”
THE QUICK ANSWER: We do not yet know if SARS COV-2 can get to the brain (cross the blood brain barrier), but we have some evidence that more people are experiencing neurological and psychiatric issues (anything affecting the brain and behavior) after having COVID-19 and EARLY evidence of brain changes after having COVID-19.
🙋 Does SARS CoV-2 cause symptoms in the brain?
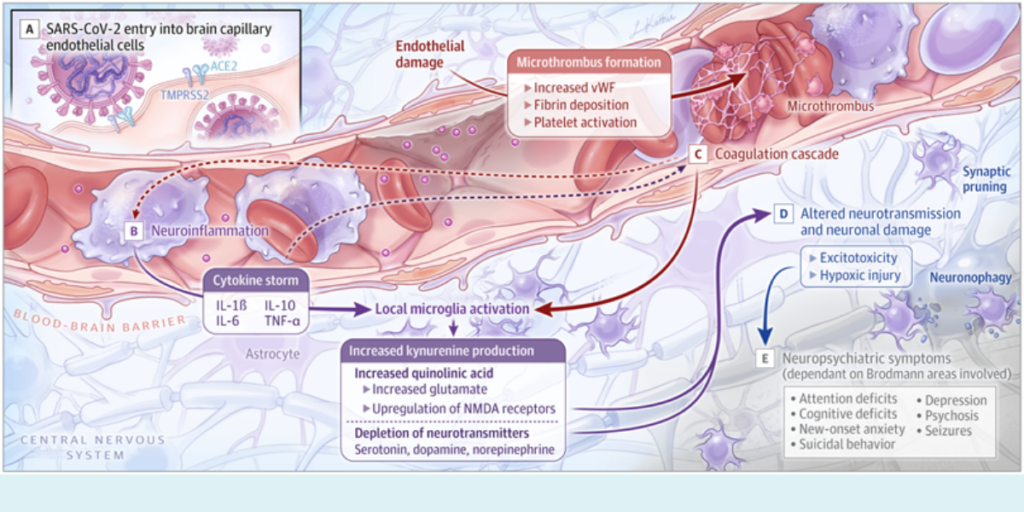
Scientists began to examine the potential mechanism of SARS CoV-2 entering into the brain because more people are reporting anxiety, depression, insomnia, psychosis, and even suicidal thoughts after COVID-19 disease. Among people who have survived COVID-19, many have reported extended difficulty with cognition, fatigue, smell, balance, and nausea, all of which may have to do with the brain. We also know that more people are having strokes and stroke-like events due to clots formed in small blood vessels leading to the brain. These clots can then cut off blood supply and oxygen to key areas of the brain involved in regulating our mood, wakefulness, sleep, balance, and senses. But, the exact mechanism of how psychiatric symptoms emerge is unknown. SARS CoV-2 could get in to the brain through damage to the blood brain barrier or through monocytes (part of your innate immune system, which may take in the virus, but then be unable to get rid of it-thus transporting it to the brain).
🧠 The brain may be affected directly by the virus, but we do not have much evidence for this. One study looked at people’s brains after they died of COVID-19 (most or all had severe illness)-changes were noted. There are many variables that could influence these changes, including lack of oxygenation, other illnesses, critical illness, and COVID-19 related sequelae (such as micro clots). So this study may not provide direct evidence as the people who died may have had more severe disease and/or other health issues which could have confused the picture (https://tinyurl.com/yh8c9vmc). This recent preprint (not yet peer reviewed), which followed people before and after COVID-19, suggests that COVID-19 results in decreases in gray matter (where most of the neurons are)-specifically in areas of the brain related to smell and taste. This makes sense since this is where the virus can enter the body itself (through the nose and mouth). But, it does not necessarily explain the onset of psychiatric symptoms after infection.
Even if we don’t know the mechanism by which this occurs, it is clear that the virus affects many systems in the body and can have long lasting impacts. Other viruses also have evidence for causing neurological and psychiatric symptoms by lingering in the body and affecting neurons and the immune system; an example of such a virus is the poliovirus-which can cause neurological symptoms in some, but not all.
🕵️ Some evidence: There appears to be an increased risk for mental health symptoms among those who have had COVID-19.
Data is still emerging, but a recent study in the Lancet that matched groups (compared two groups with similar characteristics who either had COVID-19, respiratory infection or influenza) and followed them for 90 days suggests that COVID-19 increases the risk of new onset psychiatric symptoms (nearly double) with the most common diagnoses being anxiety, insomnia, and depression. Psychosis was reported, but there was no evidence that this was related to COVID-19 infection. Dementia was also common after COVID-19 infection, although further research is needed to understand why. Of note, there may be unmeasured factors (social and economic) which may explain some of these differences. It is also important to note that the data were already collected and then analyzed and came from hospitals, primary care settings, and specialty care organizations. Follow up data at six months showed similar results, suggesting that people who have had COVID-19 may have an increased risk of psychiatric symptoms. Interestingly, how sick you are (severity of disease) does not seem to play a direct role in the onset of psychiatric symptoms. BUT, having a previous psychiatric diagnosis is likely associated with an increased risk of having psychiatric symptoms after COVID-19 disease.
😶🌫️ Of course, some people don’t experience any of the studied symptoms, but do experience brain fog. Up to 30% of people who have recovered from COVID-19 suffer from memory loss, difficulty with concentration, and cognitive fatigue-some defining features of what people call brain fog. These symptoms are NOT only present in people who have had severe illness or stroke like we would expect, but in others who have had milder illness as well. The mechanism behind this is not yet well understood but is thought to have to do with inflammation and the body attacking many cells, including some of those in the brain that are responsible for control of memory, attention, and other activities.
THE BOTTOM LINE:
✅ So to answer the question, some people will have neurological and psychiatric symptoms after COVID-19. Specifically people who have had psychiatric symptoms prior to COVID-19 are more likely to have symptoms after having COVID-19. It is likely that this does not have anything to do with how severe their disease is. And some symptoms, like “brain fog,” can linger for up to six months or more. Some people will also have anxiety, depression, or PTSD like symptoms after having COVID-19. In fact, it is well known that many people experience psychiatric symptoms after critical illness. Having COVID-19 does not mean you WILL have psychiatric symptoms-but it is common (about 1 in 3 will have symptoms after having COVID-19) and the risk appears to be higher compared to other psychiatric symptoms after other infections like influenza.
While this sounds disheartening, the important thing is to raise awareness around the possibility that someone can experience psychiatric symptoms so that people can seek help if these symptoms arise. Talk to your primary care provider if they do. The treatments are often similar to those available for traumatic brain injury and focus on periods of rest/work and building up stamina to regain function. They often involve occupational therapy as well as supportive therapy, cognitive behavioral therapy, and medications specific to the symptoms.
We are hopeful that greater awareness around this will help more people get the care they need. Thank you for your question!
With Love,
Those Nerdy Girls
If you or someone you know is considering suicide, contact the National Suicide Prevention Lifeline at 1-800-273-8255 (Español: 1-888-628-9454; Hearing Support: 1-800-799-4889) or the Crisis Text Line by texting HOME to 741741.