Short answer: We don’t know yet.
Long answer: A study by DNA testing company 23andMe recently made headlines, reporting that people with blood Type O were up to 18% less likely get infected with COVID19 than other blood types (A, B, and AB), and they were also less likely to be hospitalized. The findings appear to align, in general, with results from the few other studies available from China and New York City, and most recently from a study in Europe.
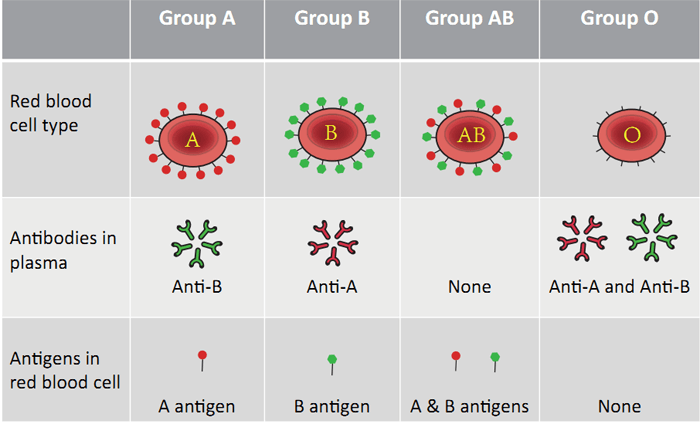
BACKGROUND: Blood type has previously been correlated with susceptibility to both infectious and chronic diseases. The blood type gene is located on a stretch of DNA that regulates inflammation and blood clotting. These processes contribute to the development of heart disease, but they also play a role in severity of COVID19. In addition, this stretch of DNA that encodes blood type is also located near the region that encodes the ACE2 protein, the receptor for the SARS-CoV-2 virus. However, it’s unknown if the genes for blood type have any bearing on ACE2 receptors in any way.
How strong is the evidence so far? We need to keep a few things in mind:
(1) Only one of these studies has been peer-reviewed or published yet. In fact, the results reported by 23andMe came in the form of a blog post on the company’s website, and have yet to be subjected to formal critique by other scientists.
(2) Because of the way these studies were designed, we can only conclude that there is a correlation between blood type and COVID-19 infection (and in the 23andMe study, it is SELF-REPORTED infection), so we simply don’t have evidence that blood type actually increases (or decreases) infection risk. Similarly, we don’t have hard evidence that a particular blood type worsens disease severity. In the published study among critically ill hospitalized COVID-19 patients from Italy and Spain, patients with blood type A had a greater odds of respiratory failure. But in the study in New York City, there were no differences in rates of intubation nor death across blood types among hospitalized patients.
So does this mean people with type O blood can get a hall pass, while the type A’s remain in detention?
That’s a hard NO! Even if these studies had been designed in a way that allowed us to conclude that blood type O reduces one’s risk of infection (or reduces risk of severe disease), this “protection” was hardly absolute. In all studies, people with blood Type O still got infected with COVID19, and a considerable proportion had poor outcomes. Alternatively, not all people with blood type A were infected, and not all progressed to more severe disease if they were sick.
As per Dr. Charlotte Houldcroft at the University of Cambridge, “each variant found here only increases a person’s risk a little bit, and we have no idea how. It doesn’t allow us to predict who will be a severe case, and it doesn’t open up any treatment options. However, it does give us a plausible place to start looking.”
Several studies are underway to investigate the genetic variants that influence COVID-19 infection and severity. In the meantime, please continue to follow social distancing guidelines to reduce risk of infection and transmission….regardless of blood type!
LINKS:
Published European study on blood type and respiratory failure
Overview of all studies on blood type and COVID-19