Q: We know that individuals in jails and prisons are disproportionately getting COVID-19. What are the reasons for this and what can be done about it? How much more likely are incarcerated people to get COVID-19 than the rest of the population?
A: Incarcerated individuals are approximately 5 times as likely as the general population to get COVID-19.
People who are incarcerated have, by definition, little control over their physical environment; therefore, they cannot effectively protect themselves from COVID-19 infection, as they are required to live in high-risk, high-density conditions. Our prisons, jails, and other carceral facilities remain seriously overcrowded, and they were not designed to permit effective social distancing even under normal conditions of crowding. In addition, many incarcerated individuals have other risk factors including underlying conditions (e.g., asthma, diabetes) and sociodemographic characteristics (e.g., incarcerated individuals in the US are more likely to be poor and Black or Brown) that make them vulnerable to both infection and severity of the disease. Correctional officers are often the individuals who bring coronavirus into the prisons, as they move in and out of the environments daily, and, in turn, outbreaks among incarcerated populations can spread to corrections officers and the surrounding communities. As of November 2020, 40 out of the US’s 50 largest outbreaks have occurred in prisons (see Lancet article below).
This quote from a recent NPR story sums up the situation (see below for full story):
“Prisons are vectors of disease, as are jails,” says Pamela Metzger, director of the Deason Criminal Justice Reform Center at Southern Methodist University’s law school. “They are filled with people who enter with preexisting health conditions, many of which may be undiagnosed. You have cramped living conditions with exceptionally poor nutrition. Ventilation is problematic in many places. You have limited access to medical care.”
The Marshall Project provides detailed state-by-state information on COVID-19 in prisons over time. We recommend you check it out.
WHAT CAN BE DONE TO REDUCE TRANSMISSION AND DEATHS IN PRISONS?
Mitigation strategies for reducing transmission in prisons include many tips we’ve provided before: increase testing and contact tracing; follow recommended quarantine and isolation protocols; improve ventilation; provide sufficient PPE for everyone; boost cleaning and handwashing practices; and facilitate social distancing. Finally, widespread immunization will be crucial here (see next question). Unfortunately, many of these mitigation strategies are not being employed.
At a more structural level, states can prevent transmission of COVID-19 in prisons and jails by decreasing the size of their incarcerated populations. This can be done in several ways. First, the number of newly arrested individuals can be reduced by issuing citations instead. In addition, individuals that are at high risk of complications from COVID-19 and/or low risk of reincarceration (e.g., older or immunocompromised individuals, people with non-violent offenses, those eligible for parole) can be granted early release. Another key strategy is to continue the hard work to undo the systemic racism that has led to a disproportionate number of Black, Brown, and poor people in prison.
WHERE DO PRISONERS FALL IN THE VACCINATION PRIORITY LINE?
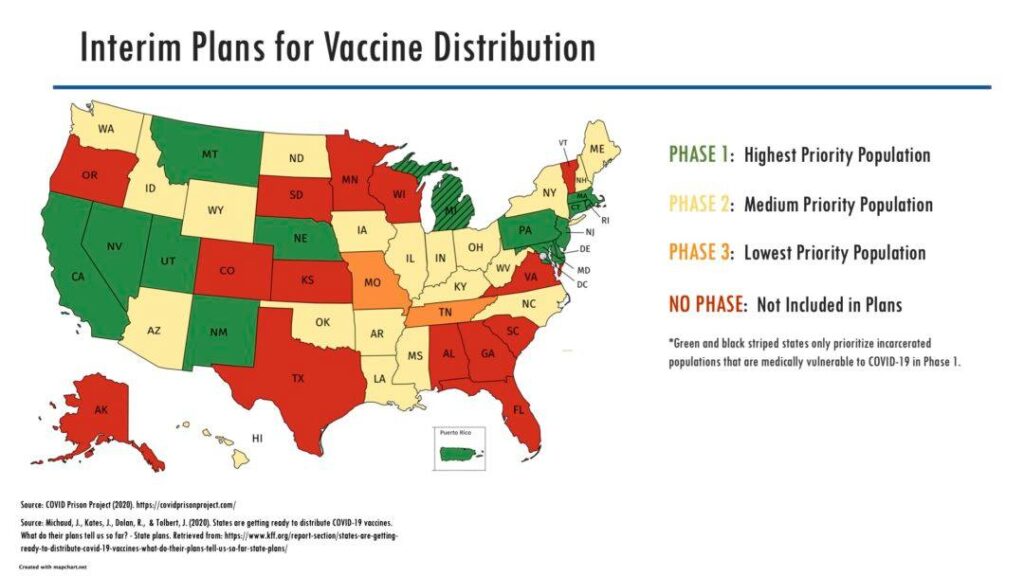
Initially, incarcerated people were not deemed a priority population for receiving the vaccines, but more recently states have moved in that direction. See the graphic above and these articles below which summarize how states are prioritizing incarcerated populations and corrections officers. These data are changing over time.
Recommendations for Prioritization and Distribution of COVID-19 Vaccine in Prisons and Jails
FINALLY, ARE ANY NERDY GIRLS WORKING ON THIS ISSUE?
Several of the Nerdy Girls are doing important work in this area.
At the request of the Dane County, WI Sherriff’s office, Dr. Jones is working on an analysis on the effects of an effort to decarcerate the county jail. The Sherriff reduced the in-jail population by nearly 40% when the COVID-19 pandemic first hit Wisconsin, a move that has substantially reduced the person-hours of exposure to COVID-19 in that setting. Dr. Jones is also engaged in public health advocacy to include incarcerated people in phase 1b of the vaccine rollout in her state.
Dr. Simanek has co-authored public health declarations which have been used by ACLU WI and others advocating for decarceration as a means to protect incarcerated persons, correctional staff, and Wisconsin communities from COVID-19. These declarations have also been used by the public defender’s office and private attorneys doing early release advocacy related to COVID-19 vulnerability.
Finally, Nerdy Girl Dr. Aronowitz wrote an Op-Ed about what is needed to help reduce COVID-19 transmission after incarcerated people are released.
Articles and websites for further reading:
Prison Policy Initiative re Overcrowding