PSA testing is the most common way to help detect prostate cancer. Screening typically begins between ages 40 and 50, but there is no universal guideline. Talk to your clinician to find out the right time for you. The earlier we detect prostate cancer, the better.
You might’ve heard in the news about former President Biden’s recent prostate cancer diagnosis. Understandably, many folks around these Nerdy Girls have been wondering about their own prostate cancer risk. Some even feel confused or anxious, and many have questions about when to get screened.
So, what exactly is prostate cancer?
Prostate cancer is one of the most common cancers. About 1 in 8 men and those with prostates will be diagnosed during their lifetime, and it is the second leading cause of cancer-related death in this group, following lung cancer [archived link]. Most prostate cancers are caused by adenocarcinomas, a type of tumor that starts in gland cells.
🤓Nerd Alert!
The prostate is a gland in the male body, usually the size of a walnut.
It is found below the bladder and in front of the rectum, and its main job is to help make some of the liquid that comes out as semen during ejaculation. This fluid helps sperm move and stay healthy.
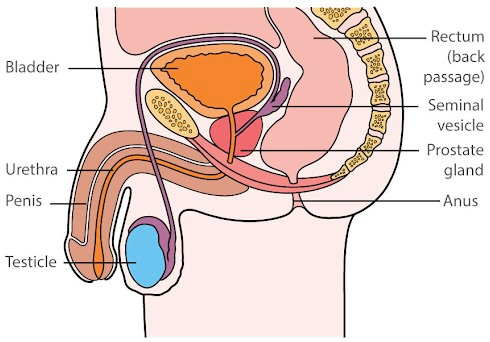
Image Credit: Male Reproductive System Macmillan Cancer Support
Prostate cancer is generally diagnosed in those 65 and older, but in rare cases it may appear in people under 40. Although about 2 in 100 people with prostates will die of the disease, the good news is that more than 99% of people with prostate cancer that has not spread past the prostate gland can live at least 5 years after their diagnosis, and some will be completely cured. However, if the prostate cancer has spread to other parts of the body outside the pelvis, the chance of living for 5 more years drops to 37%. Keep in mind that these are only general statistics. What the numbers do clearly show is that prostate cancer is very treatable when caught early.
What are the risk factors for prostate cancer?
Some of the most common risk factors for prostate cancer include:
- Older age (i.e., being 65 and above)
- Being of Black/African descent
- Family history of prostate cancer: This more than doubles one’s risk, especially if a brother (more so than a father) was affected. The risk is higher with more than one affected relative or if they were diagnosed younger than 55 years old.
- Family history of certain cancers, including breast, ovarian, pancreatic, or colon cancers.
What are the symptoms of prostate cancer?
One of the challenges of prostate cancer is that it often causes no symptoms in the early stages. When symptoms do appear, they may overlap with non-cancerous conditions like benign prostatic hyperplasia (BPH, a non-malignant enlargement of the prostate gland) or prostatitis (inflammation of the prostate). Still, any of the following symptoms should prompt a visit to your primary care clinician or urologist :
- A need to pee more frequently and/or having to pee more often at night
- Difficulty starting or maintaining urination without interruptions and/or having a weak stream of urine
- Trouble getting or maintaining an erection (erectile dysfunction)
- Blood in urine or semen (may look light pink)
- Pain while peeing, sitting, or ejaculating (releasing semen from the penis)
- Loss of bladder or bowel control
- Pain in the hips, back, or chest (which may point to cancer that has spread)
When and How Do I Get Screened for Prostate Cancer?
The most common form of screening is a PSA, or prostate-specific antigen, blood test. PSA is a protein made by both healthy and cancerous prostate gland cells. If a cancer is growing in the prostate, the PSA number may be higher than expected. But a higher number can be caused by other things too, which is why a high PSA does not necessarily mean cancer.
The typical PSA range for average-risk people is based on age.
- For people under 60: 2.5 mg/mL or lower
- For people over 60: 4.0 mg/mL or lower.
📝PSA tests alone can’t tell you if you have cancer. If your PSA is high, your clinician can suggest what next steps to take. [archived link]. They’ll likely suggest repeating the test to see if the number comes back down. They may also order other types of tests (eg. prostate MRI [magnetic resonance imaging]) or refer you to a urologist (a clinician who specializes in urinary issues).
The American Urological Association recommends that all men 50 and older talk with their clinician about PSA testing. Men with a higher risk of prostate cancer (eg, Black/African descent, first-degree relative[s] with prostate cancer) should start the discussion sooner — by age 45, or even 40 (depending on risk level).
A digital rectal exam (DRE) can also help screen for prostate cancer [archived link], but it’s less effective than PSA testing and is not the primary method recommended for prostate cancer screening. Your clinician performs a DRE by checking for lumps or hard spots in the rectum using a gloved, lubricated finger. As with any procedure, you can always decline this exam. However, it’s important to tell your clinician about any rectal symptoms you may be having.
Are there any limitations with PSA screening?
Yes. According to the American Urological Association, PSA tests can produce up to 70% false positives (a result that suggests there is cancer, even though cancer isn’t actually present). Even in those with high PSA levels, only about 25% of prostate biopsies confirm cancer. That’s why there’s no set PSA level that definitely shows you have cancer.
Sometimes, prostate cancer treatment following a cancer diagnosis can do more harm than good—especially if the cancer is slow-growing and unlikely to cause problems. The US Preventive Services Task Force’s recommendation is to stop screening around age 70, especially if you have serious health issues (heart disease, dementia, other cancers) or a life expectancy under 10 years [archived link]. At age 70, 1 in 11 men or people with prostates may have prostate cancer, but these cancers often have low Gleason* scores, and active treatment could do more harm than good [archived link]. For folks who want to learn more about cancer over diagnosis and over treatment, fellow Nerdy Girl Dr. Sarah Coles has written a great article about this HERE.
🤓 Nerd Alert!
The Gleason score is a system clinicians use to describe how aggressive prostate cancer is. This score is used in combination with PSA values and degree of disease spread (metastases) to grade the severity of the prostate cancer as low risk, (un)favorable risk, or high risk. It’s based on how cancer cells look under a microscope compared to normal prostate cells 🔬.
What the Scores Mean:
- 6 – Cancer cells look more like normal cells. The cancer is likely to grow very slowly.
- 7 – Cancer may grow slowly or moderately.
- 8 to 10 – Cancer cells look very different from normal. The cancer is more aggressive and likely to grow and spread quickly.
🤓 Nerd Alert: Research Matters
Despite the stakes, the 2025 federal budget proposes a 31% cut to National Cancer Institute funding [archived link]. This would be a major setback for prostate cancer research—just when we need better tools to distinguish harmful from harmless disease. Investing in research saves lives.
Bottom Line: Early detection is important, and PSA testing remains a valuable tool.
PSA is the most common form of screening for prostate cancer. While PSA testing isn’t perfect, it remains our best way for early detection. Yearly screening is often recommended for those ages 50 to 70, or earlier if they have additional risk factors. Ignoring abnormal results risks missing aggressive cancers that might be curable if caught early. Shared decision-making between patients and clinicians ensures that the right people are screened at the right time.
Stay well, and stay informed.
Love,
Those Nerdy Girls


