A. Recent data across U.S. states show that Black Americans and other people of color experience much higher mortality from COVID-19 than whites. Studies also point to structural barriers, and not biological susceptibility, that contribute to worse disease progression and higher mortality in these groups of Americans.
We’ve previously posted on the U.S. death toll due to COVID-19. But it’s also important to emphasize that some Americans face an even higher risk of death than others, regardless of age.
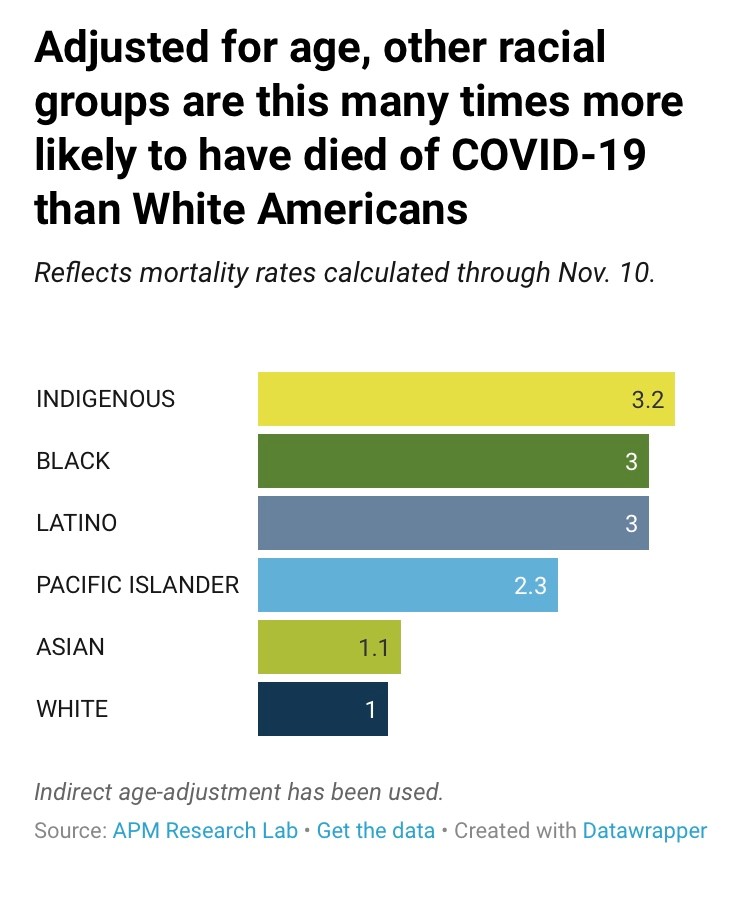
Data extracted from state department of health websites in early December show that the percentage of Black deaths due to COVID-19 is larger than the population estimate of Black people in almost every state reporting these data. When accounting for differences in the age distribution across groups (since older age confers a greater risk of death), Black, Indigenous and Hispanic/Latino Americans all have a COVID-19 death rate that is *3* times higher than White Americans.
We previously reported that COVID-19 deaths are likely UNDER counted and that analyses of excess mortality can address challenges around accurately classifying COVID deaths. Sadly, even these analyses show a much higher burden of excess deaths in people of color.
Percent of excess death compared to previous year (see CDC report):
➡️Hispanic/Latinos: 53.6%
➡️Asians: 36.6%
➡️Blacks: 32.9%
➡️Whites: 11.9%
*****Why is this happening?*****
The answer is complex but recently published studies point to structural factors, especially access to healthcare. Communities of color have the highest estimates of being uninsured, which means they are less likely to go to a doctor or hospital once sick to receive appropriate treatment.
But once individuals are admitted to a hospital, studies show no observed differences in COVID-related mortality by racial/ethnic groups. In other words, there did not appear to be any inherent susceptibility to worse COVID outcomes once individuals were receiving care.
Beyond access, there’s also evidence that communities of color have received less TIMELY care. The Lancet article below includes data on time to admission from symptom onset by race/ethnicity:
➡️For white patients, the median delay was 3 days of symptoms
➡️For Hispanics/Latinos it was 5 days
➡️For African Americans, it was 7 days – more than twice as long as whites.
Although the study was not designed to assess the reasons for the delay, other researchers have pointed to poor insurance coverage (and high out-of-pocket costs) that prevent people from seeking care early on, and a justified fear and mistrust of the healthcare system because of historical medical exploitation. This has implications for COVID outcomes, including mortality, since the available treatments for COVID work best when administered early.
BOTTOM LINE:
Some groups of Americans face a much higher risk of death from COVID-19, but there is little evidence to indicate this is due to greater biological susceptibility. More than anything, poor access to healthcare appears to be a major driver of disparities. Moreover, as Dr. Tenya Blackwell from the Ashe Institute for Urban Health notes in the linked Gothamist article, “the healthcare system also needs to build up trust and respect from its most vulnerable patients, so they can feel safe seeking help.”
LINKS:
Data on racial/ethnic disparities in COVID-19 mortality:
Our previous posts on COVID-19 death toll:
Studies on race/ethnic differences in COVID-19 mortality among hospitalized patients:
Related news articles: