Managing osteoporosis begins with lifestyle approaches. Medication can further lower the chance of a bone break from osteoporosis. Your clinician can help you decide which treatment is right for you.

When my mom was first diagnosed with osteoporosis, she was both surprised and upset. The idea of thinning bones is an unsettling thought. It’s especially hard to accept the diagnosis when you feel perfectly fine, though noticing the bit of height loss was a reality hard to ignore.
A maze of misinformation and confusion came next as my mom tried to learn about osteoporosis and figure out which treatment approach would be right for her. Online discussions often made it sound like you had to choose between lifestyle and medication, when in fact, a combination of approaches is the standard of care. She encountered “experts” touting the perfect diet, supplement, or exercise solution to “fix” her bones. Mixed in were stories of awful side effects from osteoporosis medications. Armed with what she had found online, she went to her doctor, hoping for clarity. Instead, she left even more confused, having received different advice from different doctors and struggling to keep all the medication names straight.
The truth is there’s no single best way to manage osteoporosis. Treatment is individualized, and your plan may change as your body changes or as new treatments or information become available. Affordability and insurance coverage are also factors. Knowing your options can help you discuss them with your clinician, so you can work together to find the best way to care for your bones.
Osteoporosis [archived link] is a lifelong condition in which bones become thinner and less dense, making them more likely to break (fracture) [archived link]. If your bone scan shows bone loss that isn’t as severe as osteoporosis, you may be diagnosed with osteopenia.
The main goal of osteoporosis management is to prevent painful fractures and to maintain (or even improve) mobility and function.
Lifestyle treatment approaches are essential for everyone. Your clinician may also prescribe osteoporosis medication to further help slow bone loss and strengthen your bones.
✨Learn about lifestyle approaches to managing low bone mass in this TNG post.
If you’ve been diagnosed with low bone density or thinning bones, ask your clinician to explain what might be causing yours. Some people have “secondary” causes of osteoporosis [archived link] — low bone density that’s caused by something other than older age or menopause. Your clinician may order tests to check for other causes of low bone density. This will help them decide which treatment to recommend.
👉 This post focuses on menopause and age-related osteoporosis treatment.
➡️ WHEN ARE OSTEOPOROSIS MEDICATIONS CONSIDERED?
Osteoporosis medications lower the chance of bone breaks (fractures). They’re prescribed to people who are at higher risk. Your clinician may suggest you consider osteoporosis medication if you:
- Have osteoporosis
- Have osteopenia and a high fracture risk
- Have had a hip or spine fracture after falling from standing
While there’s no crystal ball to know for sure whether you’ll break a bone, there are a number of evidence-based approaches to estimating your risk. Your clinician may consider your:
✅ T-score: A measurement of bone density found from a DEXA (or DXA) bone scan.
✅ FRAX score: Anyone can use this online calculator to estimate their chance of having a major bone break over the next 10 years. It bases the estimate on 12 different factors, including age, sex, smoking, family history, etc. Although you can calculate a score without entering your bone mineral density (BMD)—a measurement included with your T-score on your DEXA report—your FRAX score may be more accurate if you do.
✅ Personal factors and lifestyle: Your FRAX score doesn’t consider all factors that can affect your fracture risk. Diabetes and having a higher risk of falls, for example, can make your bones more likely to break, but they are not part of the FRAX score.
In general, the higher your fracture risk, the more likely you are to benefit from taking osteoporosis medication. Your fracture risk can also help you and your clinician to choose a specific treatment.
➡️ WHERE DO OSTEOPOROSIS TREATMENT RECOMMENDATIONS COME FROM?
Osteoporosis treatment guidelines come from a number of nationally and internationally recognized organizations, including:
- American Association of Clinical Endocrinologists
- American College of Obstetricians and Gynecologists (ACOG)
- American College of Physicians (update)
- The Endocrine Society
Osteoporosis treatment guidelines were generally developed for postmenopausal women. The European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases recently developed guidelines specifically for men. They follow a similar approach to what’s recommended for women. Likewise, osteoporosis medications are expected to work the same in trans people, though information is very limited.
Keep in mind, treatment guidelines are just that. Your clinician will tailor treatment to your needs and preferences.
⚖️ Health Equity Alert ⚖️
Osteoporosis is often talked about as an “old person’s disease” or something that affects Asian or white women. While it’s true that these groups are more likely to develop osteoporosis, many people outside of these groups are also at risk for low bone mass too. Myths can reinforce inequities in care. Black women in the U.S. are less likely than white women to receive osteoporosis screening and treatment, even after experiencing a fragility fracture. Men, in general, are also under-screened and under-treated. Sometimes, bias might lead to over-treatment. For example, some research suggests Asian women may be more likely to be over-treated, unnecessarily exposing them to more side effects.
Another equity consideration is that most osteoporosis research has been done in older women with European or Asian ancestry. More inclusive research is needed to make sure the findings apply to everyone, so people have the information they need to make the best decisions for their bone health.
➡️ OSTEOPOROSIS MEDICATION OPTIONS
There are a dozen [archived link] FDA-approved medications approved to prevent or treat osteoporosis in people 50 and older or after menopause. They fall into two general categories:
- Antiresorptive medications decrease bone breakdown.
- Anabolic medications increase bone building.
The chart below lists some names and key points to help you discuss your options with your clinician. Just remember, this chart doesn’t cover everything, and information can change over time.
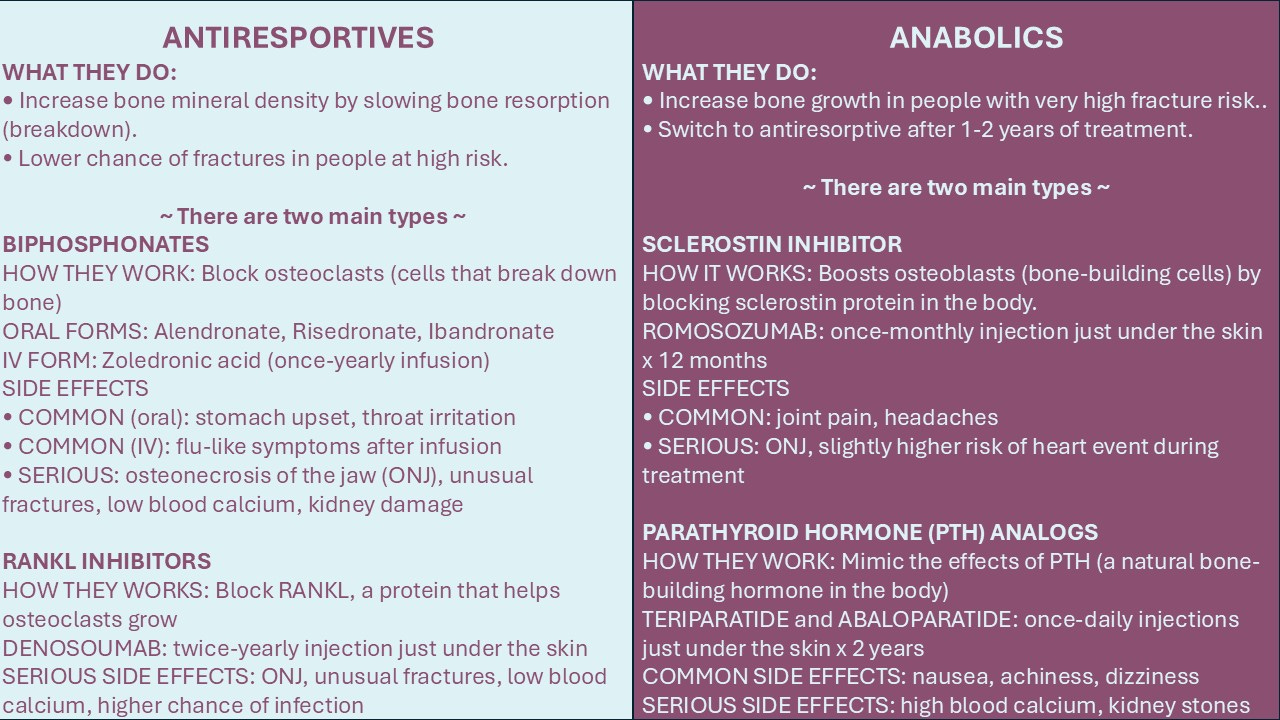
Sources: FDA-approved prescribing information for each medication (as of July 2025)
Most people are initially prescribed antiresorptive medication. But if you have a very high risk of fractures, an anabolic medication might be recommended first, followed by antiresorptive treatment.
For most people with osteoporosis, the treatment benefit from medication far outweighs the risk of side effects.
If you have osteopenia, you may also benefit from treatment if you have an additional risk factor, such as being older than 65.
Your clinician will consider your personal risk of side effects to help recommend a medication that’s safest for you.
So what are the osteoporosis medication treatment options? Let’s have a look together.
✅ Biphosphonates are a group of antiresorptive medications that are first-choice for most people. Fosamax was the first to enter the market 30 years ago. Now there are more options, and all are available as generics. Oral options include:
- Alendronate (Fosamax)
- Risedronate (Actonel)
- Ibandronate (Boniva) — Less commonly prescribed since it hasn’t been shown to prevent hip fractures.
Each medication comes in different tablet strengths that are dosed differently (i.e., once-daily, once-weekly, once-monthly). These oral bisphosphonates can cause throat irritation. In rare cases, esophageal ulcers can form. To help prevent this, be sure to follow your clinician’s instructions closely. Typically, the instructions say to take each dose with a full glass of water and not to lie down for 30 to 60 minutes afterward, depending on the medication.
✨Getting adequate calcium and vitamin D is important for everyone with low bone mass. But if you’re taking osteoporosis medication, it’s especially important. These medications help keep more calcium in your bones. So if you take your osteoporosis medication without getting enough calcium, you could end up having too little calcium in your blood, which can be serious. Make sure to follow your clinician’s diet and/or supplement recommendations closely. Learning how to add up your calcium in a day is a good idea. The USDA lists the amount of calcium in common foods here [archived link].
Zoledronic acid (Reclast) is an intravenous (IV) bisphosphonate that’s an alternative option for people who have trouble taking oral forms. It’s given as a once-yearly infusion. Some people feel achy for a few days after their infusion.
Serious risks are possible with all bisphosphonates, but they are considered rare. They include:
- Osteonecrosis of the jaw or ONJ (breakdown of jawbone)
- Atypical thigh bone fractures
- Kidney damage
- Low blood calcium
Treatment duration: Most people take an IV bisphosphonate for 3 years or an oral form for 5 years, and then start a “drug holiday” — an extended time period when no osteoporosis medication is taken. This break in treatment protects you from serious side effects. Your clinician will continue to monitor your bone density during your break from medication. If needed, they may later recommend additional treatment or switch you to a different medication.
✅ Denosumab (Prolia) is another antiresorptive option that may be recommended if your osteoporosis is severe or if you’re unable to take bisphosphonates. It’s given as a twice-yearly injection just under the skin.
Serious risks are possible with denosumab, but also considered rare. They include:
- Osteonecrosis of the jaw (ONJ)
- Atypical thigh bone fractures
- Low blood calcium
- Increased infection risk
A drug holiday isn’t recommended. Denosumab doesn’t keep working after you stop treatment like biphosphonates do. This means that stopping denosumab can lead to bone loss.
Treatment duration: Denosumab is usually continued indefinitely, unless you switch to a different medication, such as a bisphosphonate.
✅ Bone-building Medications
If your osteoporosis is severe, your clinician might initially recommend starting with an anabolic medication to help increase your bone mass. There are several FDA-approved options:
- Romosozumab (Evenity): a once-monthly injection given as two shots by a healthcare professional. Treatment duration is one year.
- Parathyroid hormone (PTH) analogs mimic the natural hormone in the body that helps build bone. Teriparatide (Forteo) and abaloparatide (Tymlos) come as once-daily injections you can give yourself at home. Treatment duration is usually no more than 2 years.
After the recommended treatment period of the anabolic medication is completed, an antiresorptive medication should be started to help your body maintain the gains in bone mass.
Anabolic medications come with unique, rare risks to consider.
- Romosozumab might increase your risk of a cardiovascular event and shouldn’t be taken if you recently had a stroke or heart attack.
- PTH analogs can cause high calcium blood levels and raise the risk of kidney stones. They have also been linked to bone cancer in animal studies, although this risk hasn’t been found in humans.
Your clinician will consider your cardiovascular and cancer risk factors when recommending an anabolic treatment.
✅ Less commonly-prescribed options
Other options your clinician may consider include:
- SERMS (selective estrogen receptor modulators) are antiresorptive hormone medications approved to treat osteoporosis in postmenopausal women. Evista (raloxifene) and Duavee (bazedoxifene / conjugated estrogens) are two options.
- Calcitonin is a natural hormone in the body that comes in a spray or injection. It’s an older medication that might be used if other osteoporosis treatments aren’t options.
Systemic forms of menopause hormone therapy (MHT) contain estrogen, which may lessen bone loss in early menopause. If you’re taking MHT to help with menopause symptoms, this may be an added benefit. But keep in mind, MHT doesn’t mean you won’t develop osteoporosis. And if you do, MHT isn’t recommended as a primary treatment for osteoporosis.
➡️ WEIGHING THE RISKS AND BENEFITS
Osteoporosis medication can help to prevent fractures. This is a big deal. Osteoporotic fractures can lead to disability, loss of function, and chronic pain that can continue for years, even after a bone break is fully healed. Additionally, the chance of dying can go up in the year following a hip fracture.
Lifespan is the length of your life. Healthspan is the portion of those years lived in good health and without disability. Osteoporosis treatment may help improve both of these measures.
But it’s also true that osteoporosis medications can cause side effects, including serious ones. That’s why osteoporosis medications are only recommended to people with a higher risk of fractures when the benefits outweigh the risks.
ONJ is by far the most notable concern people mention to me, and it’s understandable. In severe cases, ONJ can be devastating. My mom came across countless stories and photos about it online. Although disabling and painful bone fractures from osteoporosis are actually much more common than medication-related ONJ, it might not seem that way online.
To help put your own risks and benefits in perspective, here a few points to keep in mind:
✅ Consider the context
Sometimes when side effects from osteoporosis medications are mentioned online, they’re often referencing data from studies of people taking these medications for cancer (which use higher doses) or from years ago (before drug holidays became standard practice). Be aware that the information you find might make the risks seem higher than they are in your situation.
✅ Compare treatment risks with benefits
Ask your clinician to explain your side effect risks with the chance of the medication preventing you from having a fracture. Then, put the two side by side and compare.
For example, researchers estimate that bisphosphonates can prevent 8 hip fractures and 21 vertebral fractures for every 1,000 postmenopausal women treated for 1 to 3 years. For ONJ, a commonly cited risk from taking oral biphosphonates for osteoporosis is 0.01% (or one in 10,000). That would mean the risk of a hip fracture is roughly 80 times higher than the chance of ONJ. And that doesn’t include other types of fractures that can also cause long-term disability and pain.
✅ Ask if you’re more likely to get certain side effects
Make sure your clinician knows your full medical and dental history and list of current medications. This will help them know how likely you are to tolerate your osteoporosis medication. They may order blood tests too to check your kidney function and calcium levels.
If you have acid reflux or trouble swallowing pills, you’re more likely to experience side effects from oral bisphosphonates. Your clinician may recommend an IV form.
You’re more likely to develop ONJ if you have risk factors for a weaker immune system, inflammation, or infection. Some examples include:
- Gum disease or oral infections
- Cancer, diabetes or autoimmune disease
- Chemotherapy or systemic corticosteroids
- Age 65 and older
- Smoker
- Dentures
Compared with biphosphonates, some research finds that denosumab is more likely to cause ONJ, especially if taken with systemic corticosteroids.
Keep in mind, the overall risk of ONJ from antiresorptive medications is considered very low at doses used to treat osteoporosis. Your clinician can help you understand this risk and compare it with the expected benefits of treatment.
✅ Ask how to lower the chances of side effects
Learn about the potential medication side effects, including what to watch for and how to prevent them.
Follow your medication’s directions and ask your pharmacist or clinician to explain anything that doesn’t make sense.
If you’re considering a medication that can increase the risk of ONJ, here are some ways to protect yourself:
- Get a dental exam before treatment, and talk with your dentist and clinician about completing invasive dental work before starting treatment.
- Make sure your clinician knows your dental history and if you’re having any current dental or mouth issues.
- During treatment, stay up to date with dental cleanings and regular brushing and flossing.
- Let your clinician and dentist know right away if you experience bleeding gums, jaw pain, loose teeth, or trouble chewing. Catching ONJ early can decrease the risk of losing jaw bone and needing surgery.
⚖️Dental care is essential for health but often even harder to access than other healthcare. If you don’t have a dentist you can get to, get in with, or afford to see, talk with your clinician. They may know of local resources available to you. Medicare doesn’t generally cover dental care [archived link], but some people may qualify for coverage depending on their specific plan and state. For information on accessing dental care services, this article by the National Council on Aging [archived link] includes tips and resources.
✅ Consider the cost
Whether you have insurance or not, don’t assume you won’t be able to afford osteoporosis medication.
💡 Insurances typically pay for osteoporosis treatment because the cost of care is far lower than the cost of a major fracture.
Oral biphosphonates like alendronate cost about ten dollars a month (or less with insurance). The cash price of injectable medications can cost in the thousands and include clinic fees. However, that doesn’t mean the more expensive forms will have a higher out-of-pocket cost for you. For example, Medicare covers medications given in a clinic through Part B. Medicare Part D [archived link] is extra insurance you can buy to help pay for your prescription medication you take at home. Coverage and out-of-pocket costs of osteoporosis medication through Part D can vary, depending on your plan.
Your healthcare team can help you compare your costs and insurance plan. And if you don’t have insurance, they may be able to suggest other medication access options.
➡️ TIPS ON OSTEOPOROSIS CARE AND HOW TO SELF-ADVOCATE
Below are some tips for finding osteoporosis treatment:
- Start somewhere: It’s common to feel overwhelmed when managing a chronic health condition of any kind. There’s lots to think about when it comes to osteoporosis and risks from treatment. Remember, taking even one step is making progress.
- Ask for referrals and resources: Primary care clinicians often prescribe osteoporosis medication, but some people need to see specialists in rheumatology or endocrinology. Nutrition counseling and physical therapy might also help you make diet and exercise changes. Ask your clinician what resources are available to you, including where to find information and support.
- Share your concerns: If you’re uncomfortable with a specific treatment or unable to afford it, let your clinician know. They can provide more information that may ease your concerns, or they can suggest an alternative plan. You may also qualify for financial assistance or patient assistance programs through the drug’s manufacturer. It’s best to leave your appointment with a feasible plan or several options to consider.
- Know when to follow up: Osteoporosis treatment can sometimes have long follow-up periods. Add reminders so you won’t forget, and make sure to reach out sooner if you develop new skeletal pain, changes in mobility or posture, or bone injuries.
- Inform all of your healthcare providers: Everyone involved in your healthcare should be aware of your osteoporosis condition and the medications you are taking. Don’t forget to include your dentist, hygienist, and pharmacy team.
Taking good care of your bones will help them support you for years to come.
Stay strong. Stay supported. And stay osteo aware!
Further reading:
Osteoporosis drugs: Which one is right for you?
What’s the Best Osteoporosis Medication?
Comparing Osteoporosis Treatments: 9 Differences Between Boniva, Fosamax, and Prolia
At 58, I have the spine of an 80-year-old. Navigating osteoporosis has been difficult and expensive


